IMPORTANT INFORMATION ABOUT SPINE SURGERY
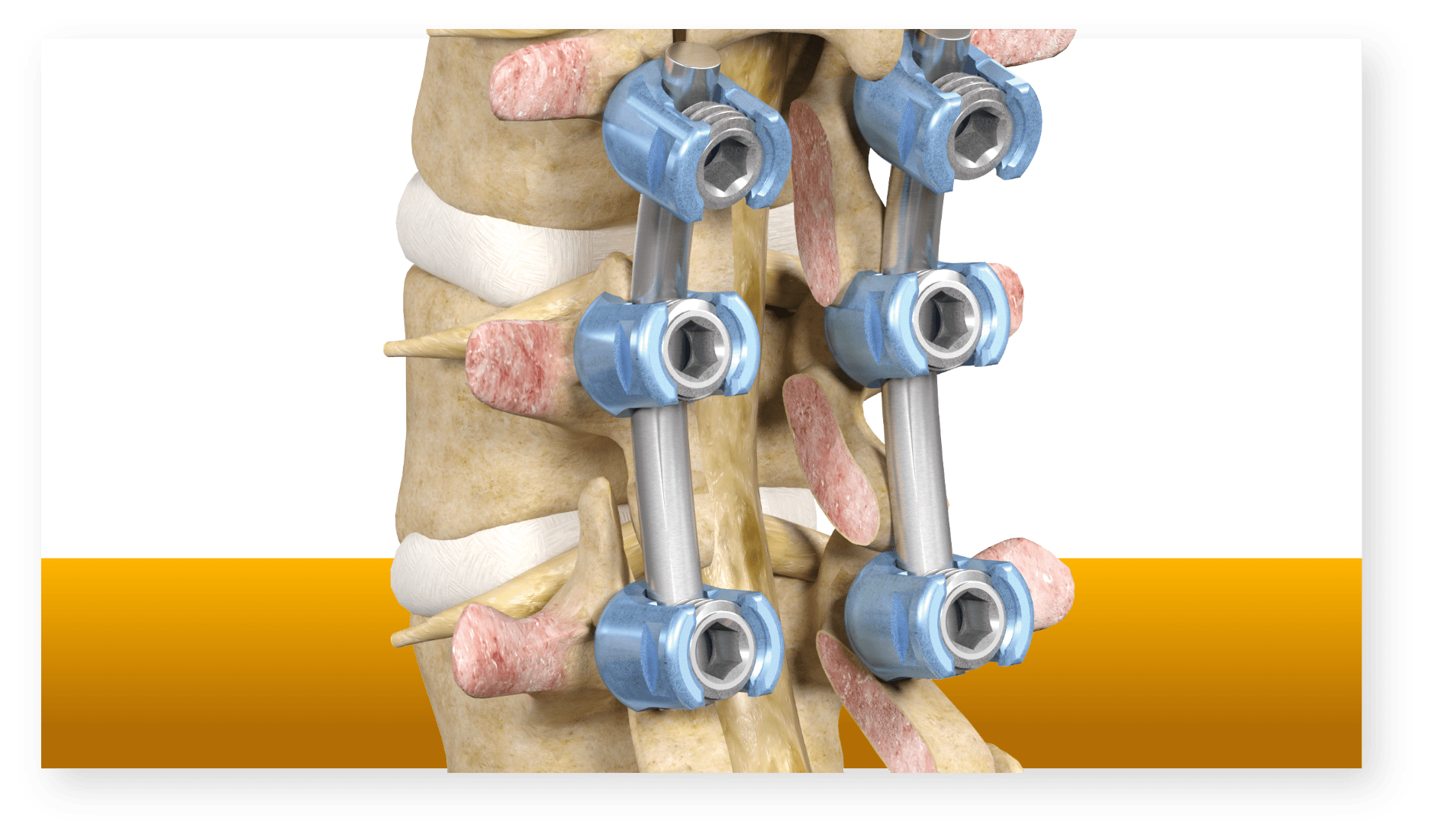
Some of the images on this website depict Stryker’s or VB Spine's products. Please speak to your doctor if you have questions about these products or anything else on this website.
Spine surgery is intended for use in individuals with the following acute and chronic instabilities or deformities of the spine: degenerative disc disease, spondylolisthesis (slipped vertebra), trauma (fracture or dislocation), spinal stenosis (narrowed space for spinal cord or spinal nerves), curvatures (scoliosis, hyperkyphosis, and/or hyperlordosis), tumor, or pseudarthrosis (failed previous spinal surgery).
Spine surgery is not appropriate for patients with any abnormality present which affects the normal process of bone remodeling (bone rebuilding) including, but not limited to, osteoporosis or osteopenia (reduced bone density), bone absorption, certain types of tumors, certain types of infections, or certain metabolic disorders; insufficient quality or quantity of bone; previous history of infection; certain types of inflammation; open wounds; a patient being overweight or obese; inadequate tissue coverage; pregnancy; a condition of senility, mental illness, or substance abuse; foreign body sensitivity (where material sensitivity is suspected); or other medical or surgical condition(s) which would preclude the potential benefit of spinal implant surgery, including, but not limited to, the presence of tumors, congenital abnormalities (birth defects) or abnormalities in red or white blood cell count.
Like any surgery, spine surgery has serious risks which include, but are not limited to, damage of the spinal cord or spinal nerves; neurological damage (damage to the nervous system); peripheral neuropathies (including pain, numbness, tingling, and/or weakness); neurovascular compromise (including loss of bowel or bladder function, or foot-drop); vascular damage; vascular disorders including thrombosis (non-moving blood clots); visceral damage (damage to organs); genitourinary disorders including kidney malfunction or failure; gastrointestinal disorders (disorders of the digestive system); bronchopulmonary disorders (disorders related to the airways or lungs) including emboli (moving blood clots); soft tissue damage; heterotopic bone formation (abnormal bone growth); bursitis (joint inflammation); heart attack; hemorrhage (blood loss); infection; delayed recovery; pain; paralysis or death.
Implant-related risks, which may lead to a revision of the device(s) include, but are not limited to, damage of the spinal cord, spinal nerves or blood vessels; fracture, fissure or perforation of the spine; wrong vertebrae (spinal bones) fused; bending, disassembly, loosening or fracture of the device(s); delay in or failure to fuse (heal); decrease in bone density; pain; discomfort; abnormal sensations; pressure on skin from components with inadequate tissue coverage, with potential extrusion through the skin; dural (spinal fluid) leak; or loss of proper spinal curvature, correction, height and/or reduction. Spinal implants may not provide the same feeling or performance characteristics experienced with a normal healthy spine. This list may not be comprehensive and/or applicable to every patient. Always speak with your doctor about the risks associated with your specific implant and procedure.
The information presented is for educational purposes only. Speak to your doctor to decide if spine surgery is appropriate for you. Your surgeon will explain all the possible complications of the surgery, as well as side effects. Each spinal surgery patient will experience a different postoperative activity level, depending on his/her own individual clinical factors. Your doctor will help counsel about how to best maintain your activities in order to recover properly from your surgery. Such activities include not engaging in high-impact activities that could de-stabilize any instrumentation that may have been implanted. It is important to closely follow your doctor’s instructions regarding post-surgery activity, treatment and follow-up care. Ask your doctor if spine surgery is right for you.
Stryker Corporation or its divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: AccuStop, Mako, SmartRobotics, Stryker. All other trademarks are trademarks of their respective owners or holders.